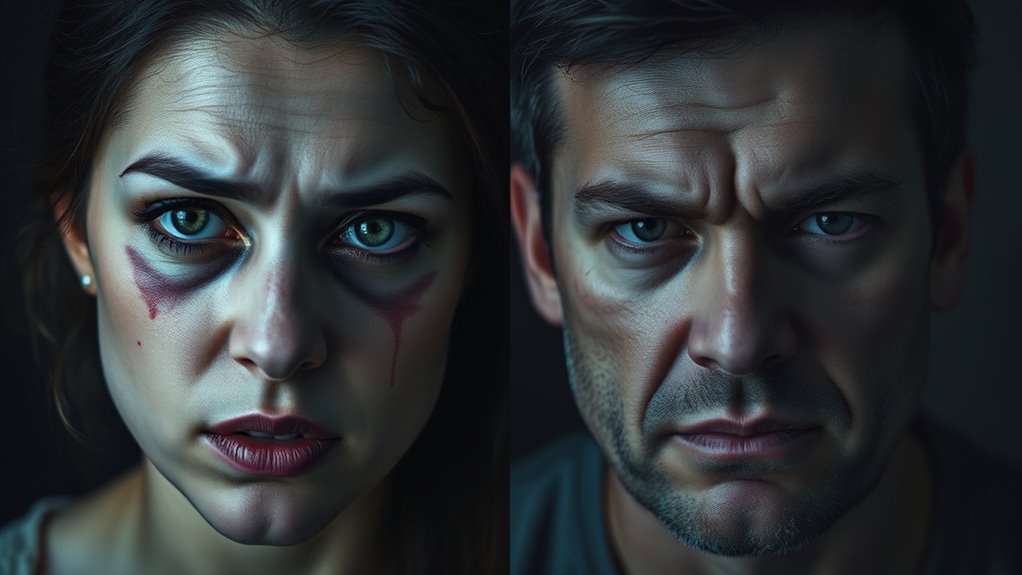
You might notice that BPD presents differently in men and women due to societal norms, trauma history, and coping styles. Women often internalize emotions, showing feelings of emptiness, self-criticism, or mood swings, while men tend to externalize, displaying impulsivity, aggression, or risk-taking. These differences can affect diagnosis and treatment. Understanding these patterns can give you a clearer picture of how gender influences BPD’s expression and what that means for care. Keep exploring to learn more.
Key Takeaways
- Women with BPD often internalize symptoms, showing emotional instability, emptiness, and mood disorders; men tend to externalize with impulsivity and aggression.
- Men frequently display externalizing behaviors like reckless risk-taking and anger outbursts, while women more commonly experience internalizing symptoms.
- Childhood trauma impacts symptom expression; physical and sexual abuse are linked to externalizing in men, emotional neglect to internalizing in women.
- Societal norms influence presentation; men may underdiagnose due to stigma and externalizing behaviors, while women are more likely to seek therapy for internal struggles.
- Diagnosis and treatment disparities exist, with men underdiagnosed and less engaged in therapy, influenced by societal expectations and clinical biases.
Gender Differences in Symptom Expression

Gender differences markedly influence how BPD symptoms manifest, shaping both clinical presentation and diagnosis. You might notice that women often display emotional instability, identity disturbances, and feelings of emptiness, leading to internal struggles. They tend to be hypersensitive to external stimuli, experiencing anxiety, avoidance, and difficulty identifying emotions, which contribute to internalizing behaviors. Men, on the other hand, frequently exhibit externalizing symptoms like impulsivity, aggression, and explosive temperaments. They may act out through anger or risky behaviors, which are more visible and often misunderstood as unrelated to BPD. While both genders experience emotional dysregulation, women’s symptoms tend to focus inward, whereas men’s external behaviors might overshadow underlying emotional issues. These differences affect diagnosis, often leading to gender biases in clinical assessment.
Internalizing vs. Externalizing Behaviors

Internalizing and externalizing behaviors are key ways that BPD symptoms present differently across individuals. Internalizing behaviors involve inward-focused struggles like intense emotional pain, feelings of emptiness, and self-criticism. You might see someone withdrawing socially, avoiding conflict, or experiencing mood swings internally. Externalizing behaviors, on the other hand, are outward actions such as impulsive aggression, anger outbursts, or reckless risk-taking. Men with BPD are more likely to display externalizing symptoms, often acting out their distress through aggression or impulsivity. Women tend to experience internalizing behaviors, showing signs of emotional sensitivity, anxiety, or despair. Recognizing these patterns helps you understand that BPD isn’t one-size-fits-all; its presentation varies based on whether behaviors are internal or external, influenced by gender and individual differences.
Emotional Sensitivity and Impulsivity

Emotional sensitivity and impulsivity are two core features that shape how BPD manifests differently across individuals. You might notice that women often experience heightened emotional sensitivity, making them more reactive to external stimuli and prone to internal turmoil. Men, on the other hand, tend to display impulsivity more openly, often acting quickly without considering consequences. Here are some key points:
- Women may internalize emotions, leading to feelings of emptiness or despair.
- Men often externalize emotions through aggressive or impulsive behaviors.
- Both genders experience intense emotions, but their expression differs.
- Impulsivity in men can manifest as reckless actions, while women may struggle with emotional regulation.
Understanding these differences can improve empathy and tailored approaches to treatment.
Patterns of Comorbid Conditions

The ways in which BPD overlaps with other mental health conditions often differ between men and women, shaping your treatment needs and experiences. Men with BPD are more likely to have comorbid substance use disorders and antisocial personality disorder, reflecting externalizing tendencies like impulsivity and aggression. Women, on the other hand, more commonly experience mood disorders, anxiety, PTSD, and eating disorders, highlighting internalizing symptoms. These patterns influence diagnosis and treatment, with men often underdiagnosed or misdiagnosed due to externalizing behaviors. Women tend to seek therapy more often, leading to higher diagnosis rates. Understanding these gender-specific comorbidity profiles helps tailor interventions, ensuring both men and women receive appropriate, targeted care to address their unique mental health challenges.
Impact of Childhood Trauma and Abuse
Childhood trauma and abuse play a critical role in shaping the development of BPD, with evidence showing that many individuals across genders experience significant adverse experiences early in life. Your early environment influences emotional regulation, attachment, and self-identity. Research suggests:
- Men often face more severe or physical forms of childhood sexual abuse, which can intensify impulsivity and externalizing behaviors.
- Women tend to experience emotional neglect or psychological abuse, contributing to internalizing symptoms like shame and identity disturbance.
- Both genders with BPD report high rates of childhood trauma, but the types and impacts differ, affecting symptom expression.
- These early adverse experiences increase vulnerability to BPD, influencing how you process emotions, relationships, and stress throughout life.
Treatment Engagement and Preferences

Your experiences with childhood trauma can influence how you approach treatment and your willingness to seek help. Men with BPD often face barriers like stigma and fear of judgment, which can make engaging in therapy more challenging. They may prefer practical, solution-focused approaches or avoid emotional discussions altogether. Women, on the other hand, tend to seek help more readily and often engage in psychotherapy and medication. Men might underutilize mental health services or drop out early, especially if they perceive therapy as incompatible with masculine norms. When they do seek treatment, they may favor interventions addressing externalizing behaviors, such as anger management or substance abuse programs. Understanding these preferences helps tailor treatment plans that encourage sustained engagement and address unique gender-related barriers.
Diagnostic Challenges and Biases

Diagnostic challenges and biases considerably influence how borderline personality disorder (BPD) is recognized and diagnosed across genders. These biases can lead to underdiagnosis in men and overdiagnosis in women. Here are some key issues:
- Gender Stereotypes: Clinicians may expect women to display internalizing symptoms, overlooking externalizing behaviors common in men.
- Assessment Tools: Many tools are designed around female symptom patterns, making it harder to identify BPD in men.
- Research Bias: Smaller male samples in studies limit understanding of male-specific presentations, skewing diagnosis.
- Stigma and Expectations: Men may avoid seeking help or be misdiagnosed with other disorders like antisocial personality disorder, complicating accurate diagnosis.
These factors contribute to inconsistent recognition, impacting treatment and understanding of BPD across genders.
Behavioral Tendencies and Personality Traits

Men with BPD often display more impulsive and aggressive behaviors, reflecting a tendency toward externalizing their emotional distress. You might notice explosive temper, irritability, and a desire for novelty or stimulation. These traits lead to risk-taking and conflict, often making their emotional struggles more visible outwardly. They may also show higher levels of anger and hostility, sometimes reacting explosively to perceived threats or frustrations. Conversely, women with BPD tend to experience heightened emotional sensitivity, despair, and internal turmoil, which manifest as internalizing behaviors like rumination or self-criticism. Both genders experience emotional dysregulation, but men often express it through external actions, such as aggression or impulsivity. These behavioral tendencies are shaped by gender norms, influencing how symptoms present and are perceived.
Response to Therapeutic Interventions

Responses to therapeutic interventions for BPD can vary markedly between genders, influenced by differences in symptom presentation, treatment engagement, and social factors. You might find that women tend to seek therapy more often and respond well to approaches like Dialectical Behavior Therapy (DBT). Men, however, often underutilize mental health services due to stigma and may present with externalizing behaviors that require tailored strategies. Consider these key points:
- Women typically engage more in psychotherapy and pharmacotherapy.
- Men show higher rates of treatment for substance use and externalizing behaviors.
- Research on treatment outcomes is often female-focused, limiting insights for men.
- Men may benefit from gender-sensitive approaches that address externalizing symptoms and stigma.
Understanding these differences helps optimize intervention strategies for both genders.
The Role of Societal Norms and Stigma

Societal expectations often influence how men and women express symptoms of BPD, with women more accepted when showing internalizing behaviors and men facing criticism for externalizing actions. Stigma around mental health can make men less likely to seek help or get diagnosed, as they may fear appearing weak or unmasculine. Recognizing these societal influences is essential to understanding disparities in diagnosis and treatment access across genders.
Gender Expectations Shaping Symptoms
Gender expectations deeply influence how symptoms of BPD are expressed and interpreted, often shaping both personal experiences and clinical perceptions. These norms can lead men and women to display behaviors aligned with societal roles, affecting diagnosis and treatment.
- Men may externalize emotions through anger or impulsivity, fitting the stereotype of masculinity’s toughness.
- Women often internalize distress, showing vulnerability and emotional sensitivity, consistent with societal expectations of femininity.
- Men might suppress feelings, making their symptoms less visible or misunderstood, leading to underdiagnosis.
- Women may seek help more readily, influenced by societal acceptance of emotional expression, which increases diagnosis rates.
These gendered expectations shape how symptoms are perceived and respond to societal judgment, impacting both personal coping and clinical assessment.
Stigma Hindering Diagnosis Access
Stigma surrounding mental health plays a significant role in preventing many individuals, especially men, from seeking or receiving an accurate diagnosis of BPD. Society often views men as strong and emotionally stoic, making it difficult for them to admit vulnerability or mental health struggles. This societal expectation discourages men from reaching out for help, leading to underdiagnosis or misdiagnosis of BPD. Additionally, clinicians may unconsciously hold biases, interpreting men’s externalizing behaviors—like impulsivity or aggression—as personality flaws rather than symptoms of a mental health condition. Fear of judgment, shame, and perceived societal expectations create barriers to diagnosis. As a result, many men suffer in silence, missing out on critical treatment that could improve their quality of life. Addressing stigma is vital to improve access and ensure equitable mental health care.
Frequently Asked Questions
How Do Gender Norms Influence BPD Symptom Expression?
Gender norms shape how you express BPD symptoms. If you’re a man, societal expectations may lead you to display externalizing behaviors like impulsivity, aggression, and anger, rather than internal struggles. Conversely, women might show more emotional sensitivity, internalizing issues like anxiety, despair, and fear of abandonment. These norms influence how you seek help, how clinicians interpret your symptoms, and how you experience and manage BPD symptoms daily.
Are There Biological Differences in BPD Between Men and Women?
You might find that about 75% of diagnosed BPD cases are women, hinting at possible biological differences. Research suggests hormonal influences, like fluctuations in estrogen and testosterone, could impact emotional regulation and impulsivity. While genetic factors may play a role, there’s still limited conclusive evidence. You should consider that biological aspects, combined with environmental influences, shape how BPD manifests across genders, but more research is needed to fully understand these differences.
How Do Societal Stigmas Affect Men’s Willingness to Seek Help?
Societal stigmas often make it harder for men to seek help for BPD. You might feel ashamed or fear judgment because expressing emotional struggles isn’t always accepted for men. This stigma can lead you to withdraw, avoid treatment, or hide symptoms, worsening your condition. Recognizing these barriers is key, so knowing that seeking help is a sign of strength can motivate you to access the support you need.
Do Treatment Outcomes Differ Between Genders?
Treatment outcomes can differ between genders, mainly because men often underutilize services due to stigma and withdrawal, which may delay recovery. Women tend to engage more in psychotherapy and pharmacotherapy, often leading to better outcomes. However, recent studies suggest that when men do receive appropriate treatment, they can experience similar improvements. Addressing gender-specific barriers and tailoring interventions may help enhance treatment success for both men and women.
Can Gender-Specific Therapies Improve BPD Management?
Imagine tailoring a key to fit a unique lock—you’ll likely see better results. Gender-specific therapies can improve BPD management by addressing distinct emotional patterns and behavioral tendencies in men and women. For instance, incorporating strategies that target externalizing behaviors in men or internalizing issues in women makes treatment more effective. Personalizing approaches helps clients feel understood, boosting engagement and fostering better long-term outcomes.
Conclusion
Understanding how BPD manifests differently in men and women helps you recognize that there’s no one-size-fits-all. Do you realize how societal norms and biases might hide or distort these signs? By being aware of these differences, you can better support those affected and encourage tailored treatment approaches. Remember, everyone’s experience with BPD is unique—so, aren’t you curious to learn more and break down the stereotypes surrounding this condition?









