BPD varies greatly across cultures, shaping how you experience and cope with the disorder. For instance, symptoms might manifest differently in collectivist societies, where fears of abandonment clash with group harmony values. Treatment also diverges; Western approaches often focus on therapies like CBT and DBT, while Eastern cultures emphasize family involvement and support. Self-harm methods differ too, with skin mutilation more common in the West and overdoses prevalent in the East. Understanding these cultural differences is key to effective care. Explore further to uncover more insights about BPD across diverse cultural landscapes.
Key Takeaways
- BPD prevalence varies greatly across cultures, with rates as low as <1% in some Chinese populations and up to 36% in Singapore.
- Cultural context influences symptom expression; collectivist societies may view abandonment fears differently, impacting diagnosis and treatment approaches.
- Treatment in Western cultures often utilizes CBT and DBT, while Eastern cultures emphasize family involvement and social support in healing processes.
- Interpersonal relationship challenges and family dynamics are significant stressors for individuals with BPD, influenced by cultural expectations and norms.
- Diagnosing BPD across cultures is complex, necessitating culturally sensitive assessment tools to capture symptoms accurately and reduce biases in treatment.
Understanding BPD Across Cultures

While understanding Borderline Personality Disorder (BPD), it's vital to recognize that its manifestations vary considerably across cultures. The cultural context plays a significant role in how symptoms are expressed and perceived.
For instance, in Eastern countries, you might notice higher rates of self-poisoning and overdose, while in Western nations, skin mutilation behaviors are more commonly reported. These variations can impact diagnosis and treatment approaches, often diverging from Western-centric criteria. Additionally, the influence of genetic predisposition and environmental factors, such as childhood trauma, can further shape the cultural expressions of BPD.
The prevalence of BPD also shows stark differences; you could find rates as low as less than 1% in some Chinese college populations, while psychiatric settings in Singapore report rates as high as 36%. In collectivist cultures, behaviors tied to BPD, like fear of abandonment, may be viewed as inappropriate due to societal values that prioritize group harmony and interconnectedness.
Moreover, symptoms such as emotional dysregulation and impulsivity are interpreted within cultural frameworks, which affects both identification and therapeutic modalities. Understanding these cultural variations is essential for accurate diagnosis and effective treatment, ensuring that you consider the broader context in which BPD manifests.
Cultural Influences on Symptoms

Cultural context shapes how symptoms of Borderline Personality Disorder (BPD) are expressed and understood. You'll notice that cultural influences greatly affect symptom expression, particularly regarding impulsivity and emotional dysregulation.
In Western cultures, individualism often leads to self-harm behaviors, while collectivist traits in Eastern cultures impact interpersonal functioning and family dynamics. Additionally, cultural beliefs surrounding health and wellness can influence how individuals seek treatment and support, with some cultures favoring natural remedies alongside conventional medications.
Here are some key differences you might find interesting:
- Impulsivity: More prevalent in Western contexts, often linked to individualistic values.
- Self-harm methods: Eastern cultures may show higher rates of poisoning, whereas skin mutilation is common in the West.
- Interpersonal functioning: Issues are frequently reported in Western cultures, while Eastern cultures focus on communal relationships.
- Prevalence rates: BPD is reported as low as 1.3% in China but can reach 36% in Singapore, indicating unique cultural factors.
- Emotional dysregulation perceptions: Societies like China may question the appropriateness of BPD diagnostic criteria, affecting recognition and treatment.
Understanding these cultural nuances can help in recognizing how BPD symptoms manifest differently across various societal contexts.
Treatment Approaches Worldwide

Understanding the varied expressions of BPD symptoms across cultures sets the stage for examining treatment approaches worldwide. In Western countries, treatment for Borderline Personality Disorder often revolves around cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT). These therapy interventions focus on individual coping strategies and emotion regulation.
In addition, the incorporation of mindfulness practices can enhance emotional regulation, a key component in managing BPD, similar to effective strategies for weight loss that emphasize mindfulness to reduce emotional eating. Conversely, Eastern cultures typically emphasize family involvement and social support, aligning with collectivistic values that prioritize community and relational harmony.
The prevalence of BPD can differ dramatically, ranging from 1.3% to 36% in various Asian countries, highlighting the need for culturally sensitive treatment approaches. Many treatment guidelines stress the importance of trauma-informed care, ensuring that practitioners recognize the impact of trauma on individuals with BPD.
To meet these diverse needs, culturally competent practitioners play an essential role, tailoring interventions to fit the unique cultural context of their patients. Research indicates a lack of robust evidence supporting the effectiveness of medications for BPD, making it essential to focus on thorough, culturally tailored therapeutic practices.
Self-Harm Methods by Region
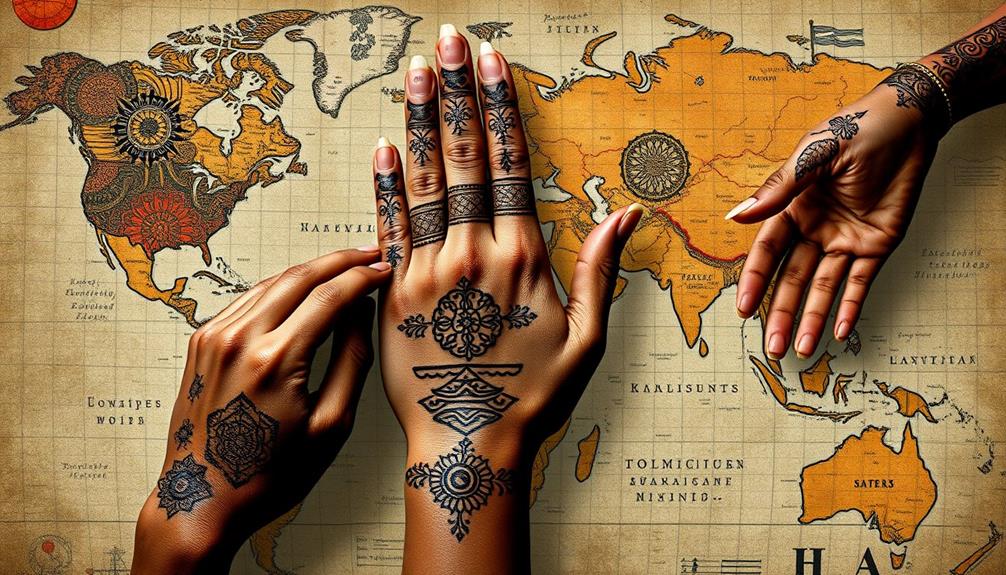
Exploring self-harm methods reveals significant regional differences that reflect cultural attitudes and social conditions. In Eastern cultures, overdose and poisoning dominate as the preferred self-harm methods, with alarming prevalence rates reaching up to 93% in areas like Sundarban, India.
Conversely, Western cultures lean heavily towards skin mutilation, especially among African Americans in Mississippi, where rates hit 77%. Understanding the financial aspects of mental health care can also play a vital role in accessing treatment, as effective interventions often require financial planning and resource allocation, similar to creating a personal budget.
Here's a quick overview of self-harm methods by region:
- Eastern cultures: Overdose and poisoning (60% prevalence)
- Western cultures: Skin mutilation (100% prevalence)
- Rural settings: Sundarban shows the highest poisoning rates
- Mississippi: Elevated skin mutilation rates
- Overall studies: 93% report skin mutilation, 71% report burning, and 62% report overdose
These cultural differences in self-harm methods highlight how BPD manifests uniquely across regions. Understanding these variations is essential for tailoring interventions and support systems that resonate with individuals' experiences in their specific cultural contexts.
Psychological Stressors in Context
When you think about Borderline Personality Disorder, it's clear that psychological stressors play a huge role in your experience. Interpersonal relationship challenges, family dynamics, and socioeconomic factors can all heighten your stress levels and contribute to self-harming behaviors.
Understanding these unique stressors in various cultural contexts is essential for finding effective support and interventions. Additionally, the financial aspects of care for those with personality disorders, including assisted living expenses, can greatly impact individuals and families seeking help.
Interpersonal Relationship Challenges
Interpersonal relationship challenges greatly impact individuals with Borderline Personality Disorder (BPD), often serving as essential psychological stressors. You might find that these challenges are deeply influenced by your cultural context, shaping how you navigate emotional turmoil and relational dynamics.
Factors such as divorce proceedings can exacerbate feelings of instability and fear of abandonment, particularly in cultures where familial bonds are emphasized.
Key factors contributing to these challenges include:
- Interpersonal problems that lead to feelings of instability and fear of abandonment.
- Family dynamics that can exacerbate stress, especially in cultures with strong familial expectations.
- Family discord consistently cited as a significant psychological stressor, affecting your emotional well-being.
- Relational challenges arising from marital conflict or parental divorce, particularly in Western cultures.
- Cultural perceptions that influence how BPD symptoms manifest and are treated across different societies.
Understanding these elements can clarify why treatment involvement often requires addressing these interpersonal issues.
In both Eastern and Western cultures, recognizing and tackling these stressors is crucial for effective intervention and support, allowing you to work through the complexities of your relationships and improve your overall mental health.
Family Dynamics and Conflict
Family dynamics greatly shape the psychological stressors faced by individuals with Borderline Personality Disorder (BPD). Marital conflicts and discord among family members often amplify interpersonal problems, increasing the risk of self-harming behaviors. When family relationships are strained, such as during a parents' divorce, you might experience heightened stress, which can worsen the manifestation of BPD.
Additionally, employing strategies to navigate partner shutdown in disputes can be beneficial in managing conflicts that arise within family settings, as it encourages open communication and understanding. For instance, using active listening techniques can help family members express their feelings more effectively.
The psychological stressors linked to family dynamics don't just stem from conflict; they can also arise from unmet family expectations. In various cultural contexts, these expectations might differ considerably, influencing how you cope with stressors. For instance, in some cultures, the pressure to conform to family roles can exacerbate feelings of inadequacy, leading to maladaptive coping strategies like self-harm.
Overall family discord is a major factor in the psychological landscape of BPD. It can trigger emotional instability and make it harder for you to find effective coping strategies. Recognizing the cultural variations in family dynamics is essential to understanding how these stressors impact individuals with BPD, ultimately shaping their emotional experiences and responses to conflict.
Socioeconomic Stress Factors
Socioeconomic stress factors greatly impact individuals with Borderline Personality Disorder (BPD), often exacerbating their psychological distress. These stressors can manifest in various ways, markedly influencing mental health across different cultural contexts.
For instance, while interpersonal problems are commonly reported in Western nations, Eastern nations often see higher rates of self-poisoning linked to socioeconomic stressors. Additionally, key domains of development such as emotional and psychological growth may be hindered by these stressors, affecting individuals' abilities to cope effectively.
Here are some key socioeconomic stress factors affecting individuals with BPD:
- Financial difficulties leading to anxiety and insecurity
- Family dynamics, such as marital conflict and parental issues
- Academic pressures, particularly among younger individuals
- Health problems and access to healthcare resources
- Experiences of abuse and violence in the community
Understanding these stressors is essential for developing effective treatments. With 52% of studies linking psychological stressors to self-harm, recognizing the role of socioeconomic challenges becomes imperative.
Culturally sensitive interventions can address these issues, helping individuals navigate their unique circumstances. By prioritizing mental health and acknowledging the influence of socioeconomic stressors, you can better support those grappling with BPD, fostering healthier coping mechanisms and improving overall well-being.
Family Dynamics and BPD

Family dynamics play an essential role in shaping your experience with BPD, as interpersonal relationships often amplify stress.
In many cases, the alignment of family values and beliefs can influence how individuals cope with emotional challenges, making astrological compatibility a pertinent factor in understanding these relationships.
If you're dealing with conflict, whether it's parental or cultural, it can greatly impact your emotional well-being.
Understanding how these dynamics interact can help you navigate your challenges more effectively.
Interpersonal Relationships Impact
Interpersonal relationships considerably shape the experiences of individuals with Borderline Personality Disorder (BPD), particularly through the lens of family dynamics. The impact of family relationships on BPD symptoms can't be overstated. You might find that psychological stressors from family discord amplify self-harming behaviors and complicate your treatment journey.
For instance, the stress of unresolved family conflicts can increase feelings of anxiety, making it harder to manage symptoms effectively. Exploring holistic approaches, such as essential oils for emotional support, may also provide additional relief in managing emotional turmoil.
Here are some key points to reflect on:
- Parental divorce often increases psychological stress, affecting your interpersonal relationships.
- Marital conflict and issues with parents or guardians are prevalent stressors linked to BPD.
- Cultural influences play a role; collectivist societies tend to emphasize family cohesion, while individualistic societies may highlight personal autonomy.
- Interpersonal problems within family contexts are more frequently reported in Western nations compared to Eastern nations, showcasing cultural divergence.
- Treatment reflections must account for family dynamics, as overall family discord can exacerbate symptoms.
Understanding how family relationships impact your experience with BPD can help you find effective treatment strategies. By recognizing the role of cultural influences and addressing family dynamics, you can work towards healthier interpersonal relationships and improved emotional well-being.
Cultural Conflict and Stress
Cultural conflict often adds another layer of complexity to the experiences of individuals with Borderline Personality Disorder (BPD). In many cases, family dynamics greatly influence psychological stressors like marital conflict and issues with parents, which can heighten self-harm behaviors.
For instance, parental divorce in collectivist cultures can lead to increased stress, exacerbating BPD symptoms. The emphasis on familial relationships in these cultures often complicates interpersonal problems, creating additional family issues that individuals must navigate.
These dynamics reveal the importance of understanding the cultural context surrounding BPD. Treatment approaches that lack cultural sensitivity may not address the unique challenges faced by individuals in different settings.
For example, while some therapies focus on individual healing, they might overlook how family expectations and relationships contribute to one's struggles. By incorporating a culturally aware perspective, mental health professionals can better support individuals dealing with BPD.
Recognizing the interplay between cultural conflict and family dynamics allows for more effective interventions, ultimately helping you manage your symptoms and improve your overall well-being.
Cross-Cultural Diagnosis Challenges
Diagnosing Borderline Personality Disorder (BPD) across different cultures presents numerous challenges that can significantly impact patient care.
Cultural biases often cloud the definition of BPD, leading to misdiagnosis or underreporting, particularly in collectivist societies where symptoms may manifest differently. The DSM-5's criteria mightn't capture these unique cultural expressions, which complicates the diagnosis.
Consider the following challenges:
- Cultural biases can skew the understanding of BPD symptoms.
- Misdiagnosis can occur due to a lack of culturally relevant assessment tools.
- Interpersonal dynamics during diagnostic interviews can change based on cultural context.
- Racial disparities exist, with Black patients diagnosed with BPD less frequently than their White counterparts.
- Limited epidemiological data from non-Western cultures makes prevalence comparisons difficult.
These factors highlight the need for a more nuanced approach to diagnosing BPD.
Recommendations for Culturally Sensitive Care

To provide effective care for individuals with Borderline Personality Disorder (BPD), it's vital to understand how local norms and values influence emotional expression and relationships.
Culturally sensitive care involves recognizing that patients from collectivist cultures may prioritize family involvement and community support in their mental health journey. As a mental health professional, you should integrate these elements into treatment plans.
Utilizing culturally appropriate assessment tools is essential for accurately capturing the unique symptomatology of BPD across diverse populations. Standard Western diagnostic criteria mightn't fully reflect the experiences of individuals from non-Western contexts.
Being aware of cultural variations in perceptions of self-harm and impulsivity can also guide your approach; behaviors that seem maladaptive in Western societies might've different interpretations elsewhere.
Training in cultural competence is critical. It equips you to engage effectively with patients from various backgrounds and helps minimize biases in diagnosing and treating BPD.
Conclusion
In the intricate tapestry of human experience, understanding BPD across cultures is like charting a vast ocean, where each wave reflects unique symptoms and treatment approaches. Just as a sailor adapts their course to the winds, you too must embrace cultural nuances in care. By fostering empathy and awareness, you can help harmonize the discordant notes of psychological stressors and family dynamics, creating a symphony of healing that resonates across borders and truly honors each individual's journey.
Theresa is the visionary force behind Borderline Syndrom, steering our content towards excellence and integrity. With a keen eye for detail and a deep understanding of BPD, she ensures that our articles, stories, and resources offer our readers valuable insights, hope, and guidance. Theresa’s leadership not only shapes our editorial direction but also fosters a space where voices on BPD are heard and respected.