You may experience co-occurring conditions like depression, bipolar disorder, anxiety, substance use, eating disorders, or PTSD with BPD, which can intensify emotional instability and impulsivity. These overlapping issues make diagnosis and treatment more complex, requiring a holistic, integrated approach. Recognizing the signs and understanding contributing factors, such as trauma or genetics, can help manage these conditions more effectively. Continue exploring to discover how all-encompassing care can improve your stability and well-being.
Key Takeaways
- Common co-occurring disorders with BPD include mood disorders, anxiety, substance use, eating disorders, and PTSD.
- Co-occurring conditions exacerbate emotional instability and impulsivity, complicating diagnosis and treatment.
- Childhood trauma, genetics, and environmental stressors contribute to the development of multiple disorders alongside BPD.
- Integrated, multidisciplinary treatment approaches are essential for managing BPD and its co-occurring conditions effectively.
- Early detection and comprehensive care improve prognosis and reduce the risk of crises and long-term complications.
Common Mental Health Conditions Co-Existing With BPD
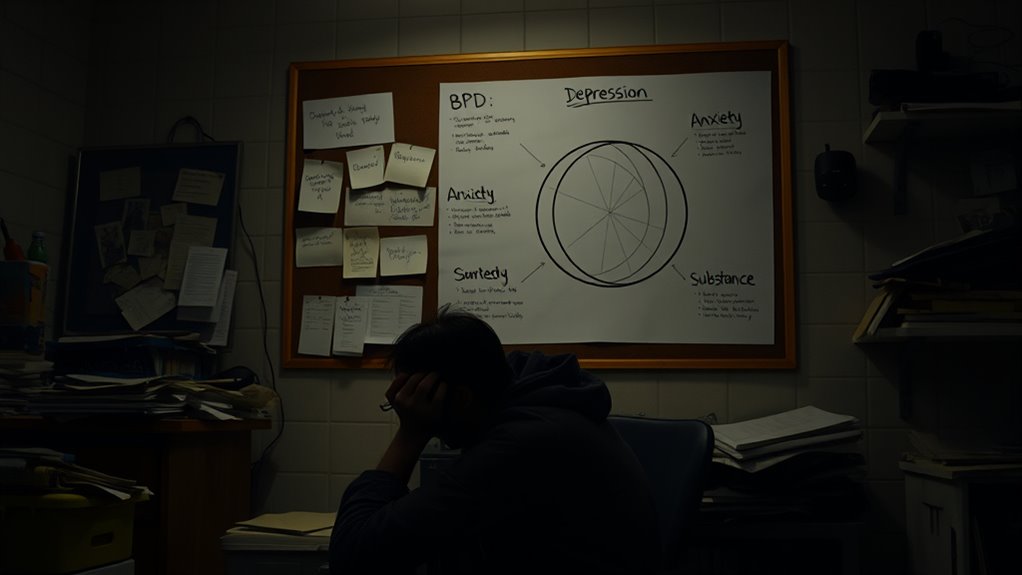
Many individuals with Borderline Personality Disorder (BPD) also struggle with other mental health conditions, which can complicate diagnosis and treatment. You might experience mood disorders like depression or bipolar disorder, leading to intense emotional instability. An accurate diagnosis often requires careful assessment of all co-occurring conditions to ensure comprehensive care.
Anxiety disorders often co-occur, heightening feelings of worry and distress. Substance use disorder affects up to two-thirds of people with BPD, frequently involving alcohol or drugs to cope. The presence of substance use can also interfere with treatment effectiveness and recovery efforts. Recognizing and addressing substance use is vital for successful management of BPD and concurrent conditions.
Eating disorders, such as anorexia or bulimia, are common, impacting up to 90% of those with BPD. Additionally, over half of individuals are diagnosed with PTSD, often linked to trauma or childhood abuse. Recognizing these overlapping conditions is crucial for developing personalized treatment plans. The complexity of co-occurring conditions underscores the need for a comprehensive and multidisciplinary approach in treatment.
These co-occurring mental health conditions create a complex clinical picture, making it essential to address all aspects for effective management and recovery. Understanding how comorbidities and other technical factors influence visual perception can help tailor more effective treatment environments for individuals with BPD.
How Co-Occurring Disorders Impact BPD Symptoms and Treatment
Co-occurring disorders considerably influence the severity and presentation of BPD symptoms, often making emotional instability and impulsivity more intense. These comorbid conditions, like mood, anxiety, or substance use disorders, increase emotional dysregulation and complicate diagnosis, leading to diagnosis challenges. Substance use can worsen risky behaviors and self-harm, impeding symptom management. Without integrated treatment, treatment outcomes often suffer, as addressing only BPD ignores the full scope of mental health disorders involved. Dual diagnosis requires a tailored approach to improve stability and reduce impulsivity effectively. Understanding these impacts helps you recognize that treating BPD alone isn’t enough; holistic care targeting both BPD and co-occurring disorders is essential for better recovery. Recognizing the influence of comorbidities on BPD can guide clinicians toward more comprehensive treatment strategies.
Recognizing the Signs of Dual Diagnosis in BPD Patients

Recognizing the signs of dual diagnosis in BPD patients can be challenging because symptoms of co-occurring disorders often overlap with those of borderline personality disorder. You need to look beyond typical BPD symptoms like emotional instability, impulsivity, and relationship issues, as they may mask or mimic signs of comorbid conditions like mood disorders or substance use. Persistent behaviors such as substance cravings or prolonged depressive episodes can signal a dual diagnosis. A thorough mental health assessment is essential, exploring behavioral patterns and history across different domains. Advances in machine learning algorithms can aid clinicians in identifying subtle patterns that differentiate between BPD and co-occurring conditions, improving diagnostic accuracy. Incorporating comprehensive diagnostic tools enhances the ability to distinguish overlapping symptoms, leading to more precise treatment plans. Understanding how lifestyle factors, such as remote work, can influence mental health and symptom presentation is also important in comprehensive evaluation. For example, building tension due to isolation or irregular routines may exacerbate underlying conditions. Additionally, considering trauma history can help differentiate between primary BPD symptoms and those stemming from other disorders. Accurate diagnosis requires identifying subtle differences and considering demographic factors like trauma history. Recognizing these signs is vital for providing comprehensive care and addressing all underlying issues effectively, avoiding diagnosis challenges and ensuring targeted treatment for both BPD and co-occurring disorders.
Factors Contributing to the Development of Multiple Disorders

Understanding the factors that contribute to developing multiple disorders alongside BPD can help you better recognize the complex roots of these conditions. Childhood trauma, abuse, and neglect markedly raise the risk of co-occurring disorders like PTSD and mood disorders.
Genetic factors and neurobiological changes, including neurotransmitter imbalances and brain structure alterations, create shared pathways that increase developmental risk for mental health comorbidity. Vetted – Mother Baby Kids Environmental stressors, such as unstable family environments and early life adversities, further influence the emergence of multiple disorders. These factors often interact, making it challenging to distinguish between conditions and complicating treatment.
Recognizing how childhood trauma, genetic predispositions, and neurobiological shifts contribute helps you understand the intricate nature of co-occurring disorders with BPD. For example, neurobiological changes can lead to brain structure alterations that impact emotional regulation and behavior, increasing vulnerability to multiple conditions. Research indicates that consistent use of exfoliating acids like glycolic acid can improve skin texture, which may also serve as a metaphor for the importance of addressing underlying biological factors in mental health. Additionally, the presence of neurotransmitter imbalances can significantly influence mood regulation and impulsivity, further complicating comorbid diagnoses. Moreover, advances in neuroimaging techniques are helping researchers better understand how brain changes underpin these interconnected disorders.
Approaches to Integrated Care for BPD and Its Co-Occurring Conditions

Effective treatment for BPD alongside its co-occurring conditions requires a thorough, multidisciplinary approach. Integrated care combines psychotherapy, medication management, and support services tailored to your unique needs.
Comprehensive, personalized care is key to managing BPD and co-occurring conditions successfully.
Evidence-based therapies like Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT) are essential for addressing both BPD and comorbidities such as substance use or mood disorders. In addition, ongoing symptom monitoring helps identify emerging issues early and adjust treatment plans accordingly. Regular assessments also facilitate the early detection of comorbid conditions, which can significantly improve treatment responsiveness. Incorporating alimony laws can also be beneficial in understanding the legal aspects of support and stability during recovery. Understanding treatment adherence strategies can further enhance the effectiveness of integrated care approaches.
Your treatment plans involve close collaboration among mental health professionals, primary care providers, and specialists to manage complex symptoms effectively.
Early detection and simultaneous intervention improve your prognosis and reduce crisis risks.
Structured programs with psychoeducation, skills training, and ongoing monitoring enhance adherence and promote long-term stability, helping you achieve better symptom management and a healthier, more balanced life.
Resources and tools can further support comprehensive care and improve overall outcomes.
Frequently Asked Questions
What Co Occurs Most Often With Borderline Personality Disorder?
You might wonder which condition most often occurs with BPD. Nearly 90% of individuals with BPD also struggle with eating disorders like anorexia or bulimia, making them the most common co-occurring issues.
These disorders often intensify emotional instability and complicate treatment. Recognizing this connection helps you understand the importance of holistic care that addresses both BPD and eating disorders for better outcomes.
What Disorders Are Linked to Borderline Personality Disorder?
You’re asking about disorders linked to borderline personality disorder. Many people with BPD also struggle with mood disorders like depression and bipolar disorder.
Substance use, especially alcohol and stimulants, is common.
Eating disorders such as anorexia and bulimia often occur alongside BPD.
Trauma-related conditions like PTSD, along with anxiety disorders like panic attacks and phobias, frequently co-occur, making treatment more complex.
What Medications Should Be Avoided With BPD?
You should avoid medications that increase impulsivity or agitation, like stimulants such as Ritalin, because they can worsen BPD symptoms.
Benzodiazepines pose risks of dependency and disinhibition, making them unsuitable for long-term use.
Be cautious with certain antipsychotics and mood stabilizers, as they might intensify emotional dysregulation.
Also, avoid sedatives or drugs impairing judgment unless closely monitored, to prevent worsening impulsive behaviors.
What Illnesses Overlap With BPD?
You might wonder what illnesses overlap with BPD. Many individuals with BPD also experience mood disorders like depression and bipolar disorder.
Substance use issues such as alcohol and drug abuse are common.
Eating disorders like anorexia and bulimia frequently occur, along with anxiety disorders like PTSD and panic disorder.
Additionally, other personality disorders, including avoidant or paranoid types, can overlap, making diagnosis and treatment more complex.
Conclusion
Understanding co-occurring disorders with BPD isn’t just about recognizing symptoms — it’s about seeing how these conditions intertwine. Some experts suggest that addressing both simultaneously could actually accelerate recovery, challenging the idea that treating one at a time is best. By adopting integrated care, you may find that managing multiple disorders becomes more manageable, empowering you to take control and foster lasting healing. Embrace this approach, and you might just discover new pathways to wellness.









