Medications for BPD target specific symptoms like mood swings or impulsivity but can’t cure the disorder itself. Its complex nature involves genetics, trauma, and environment, which no single drug can fully address. Long-term use carries risks, and medications often provide limited benefits without psychotherapy. To truly manage BPD, you need an integrated approach with therapy and support. If you want to understand why no single medication works, keep exploring these interconnected factors.
Key Takeaways
- BPD symptoms are highly variable, requiring personalized treatment approaches rather than a single medication solution.
- No existing drug addresses all core symptoms of BPD; medications target specific issues like mood swings or impulsivity.
- The disorder involves complex genetics, trauma, and environment, making a single pharmacological cure impossible.
- Medications often have limited long-term effectiveness and may carry risks, emphasizing the need for psychotherapy.
- A comprehensive treatment plan combining medication, therapy, and social support is essential for managing BPD effectively.
The Complex Nature of BPD and Its Symptoms

Borderline Personality Disorder (BPD) is inherently intricate, involving a wide range of symptoms that vary greatly between individuals. You might experience intense emotional swings, impulsivity, unstable relationships, or identity confusion. These symptoms don’t have a one-size-fits-all pattern, making diagnosis and treatment challenging. No single brain region or neurotransmitter causes BPD; instead, it results from interactions between genetics, environmental factors, and trauma. Many people also face other conditions like depression, anxiety, or ADHD, which complicate the picture further. Because symptoms differ so much from person to person, targeting BPD with medication becomes difficult. Instead, a exhaustive approach that considers these diverse symptoms is necessary, emphasizing psychotherapy and personalized care rather than relying on a single medication to fix everything.
The Limitations of Pharmacological Treatments

Medications have long been considered as a supplement to psychotherapy in managing BPD symptoms, but their effectiveness remains limited. You might find some drugs help with specific issues like impulsivity or mood swings, but no medication reliably reduces all core symptoms. Many treatments show only modest benefits and often lack long-term impact on functioning or remission. Risks, such as increased hospitalization or suicidal behavior, are linked to some drugs, especially benzodiazepines and antidepressants. Polypharmacy is common but not evidence-based, raising concerns about side effects. Most trials involve small samples and short follow-ups, so results are uncertain. Currently, no medication has FDA approval for BPD, making psychotherapy the primary treatment approach, with meds as adjuncts for targeted symptoms or comorbidities.
The Role of Medications in Managing Specific Symptoms

While no single medication can address all aspects of BPD, certain drugs can effectively target specific symptoms. For emotional dysregulation, mood stabilizers like lamotrigine or valproate may help reduce mood swings and irritability. Antipsychotics can decrease transient psychotic-like symptoms, impulsivity, and aggression in some individuals. Stimulant medications, especially for those with comorbid ADHD, have shown promise in reducing impulsivity and suicidal behavior, with some studies indicating up to a 48% decrease in suicide risk. However, these benefits are limited to patients with specific symptoms or comorbidities. It’s important to remember that medications are tools to manage targeted symptoms and are most effective when combined with therapy. They are not standalone solutions for the complex challenges of BPD.
Risks and Challenges of Long-Term Medication Use
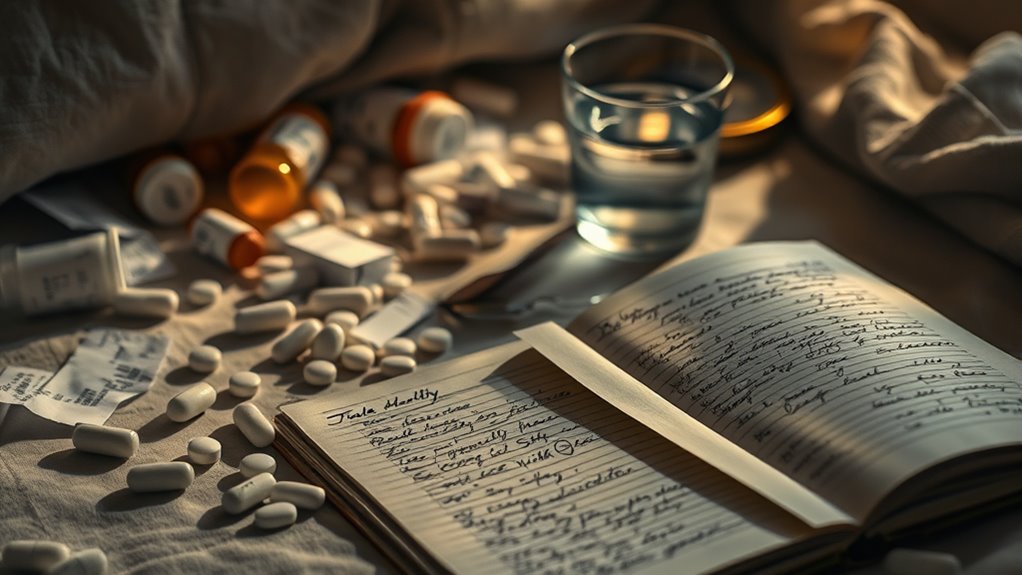
Long-term use of medications in BPD presents significant risks that can undermine treatment outcomes. Benzodiazepines, for example, are linked to increased suicide risk and worse overall prognosis. Antidepressants and antipsychotics are associated with higher rates of hospitalization, including psychiatric and all-cause admissions, without proven long-term benefits. Most medications fail to produce lasting improvements in functioning or remission, and polypharmacy often becomes the default but isn’t evidence-based. Additionally, many drugs carry side effects—weight gain, metabolic issues, cognitive dulling—that can worsen quality of life. Without large, definitive trials, it’s unclear whether these medications offer durable benefits. Relying heavily on long-term pharmacotherapy may distract from proven therapies and can pose more risks than rewards in managing BPD effectively.
The Importance of Psychotherapy and Comprehensive Care

Psychotherapy is the cornerstone of effective Borderline Personality Disorder treatment because it directly targets core symptoms like emotional dysregulation, impulsivity, and unstable relationships. It helps you develop skills to manage intense emotions, improve relationships, and build a stable sense of self. While medications may address specific issues, therapy provides lasting change through skill-building and emotional regulation techniques. A holistic care approach combines psychotherapy with social support, medication when needed, and treatment for comorbid conditions. This integrated strategy enhances your overall functioning and reduces risks like self-harm or hospitalization. Remember:
- Evidence-based therapies like Dialectical Behavior Therapy (DBT) are proven effective.
- Medications serve as adjuncts, not replacements, for therapy.
- Addressing comorbidities improves overall outcomes.
- A multidisciplinary approach offers personalized, all-encompassing care.
Frequently Asked Questions
Are There Any New Medications Showing Promise for BPD Treatment?
Currently, no new medications show definitive promise for treating BPD broadly. However, some research suggests that certain drugs targeting specific symptoms, like novel antipsychotics or mood stabilizers, may offer benefits in reducing impulsivity or emotional instability. You should know that these are still experimental and not widely approved. The best approach remains psychotherapy, with medications used as adjuncts for particular symptoms or comorbidities, pending more conclusive evidence.
How Do Medications Interact With Psychotherapy for BPD?
Medications in BPD are like sidekicks, supporting your journey alongside psychotherapy. They can help target specific symptoms like impulsivity or mood swings, making therapy sessions more productive. However, they don’t replace the skills you learn in therapy; instead, they complement it. By working together, medication and psychotherapy can create a stronger, more balanced approach, helping you manage symptoms while building healthier relationships and emotional resilience.
Can Medication Help With Long-Term Recovery or Remission in BPD?
Medication alone doesn’t lead to long-term recovery or remission in BPD. While certain drugs may reduce specific symptoms temporarily, they rarely improve overall functioning or emotional stability over time. You’ll find that psychotherapy, especially dialectical behavior therapy, remains the most effective approach for lasting change. Medications can be helpful as adjuncts for managing particular issues, but sustained recovery depends on consistent therapy, skill development, and social support.
What Are the Best Strategies to Minimize Medication Side Effects?
To minimize medication side effects, you should start with the lowest effective dose and monitor your response closely. Communicate openly with your healthcare provider about any adverse effects, and don’t hesitate to report new or worsening symptoms. Regular follow-ups help adjust medications promptly. Combining medication with psychotherapy can reduce reliance on drugs, lowering side effect risks. Always adhere to prescribed instructions and avoid polypharmacy unless advised by your doctor.
Is Personalized Medicine a Future Option for BPD Treatment?
You might wonder if personalized medicine is a future option for BPD treatment, and it definitely holds promise. Since BPD symptoms and causes vary widely, tailoring treatments to your genetics, environment, and specific needs could improve effectiveness. Advances in genetics and biomarkers may help identify which medications target your unique profile, reducing side effects and increasing success. While still in development, personalized approaches could transform how you manage this complex condition.
Conclusion
Remember, managing BPD is like tending a delicate garden—you need a mix of tools, not just a single medicine to make it flourish. Medications can help nurture specific blooms, but they can’t tend the entire landscape alone. Embrace psychotherapy and holistic care as your guiding sunlight, helping you grow stronger each day. With patience and the right support, you’ll find your path through the storm, blooming into resilience and hope.









