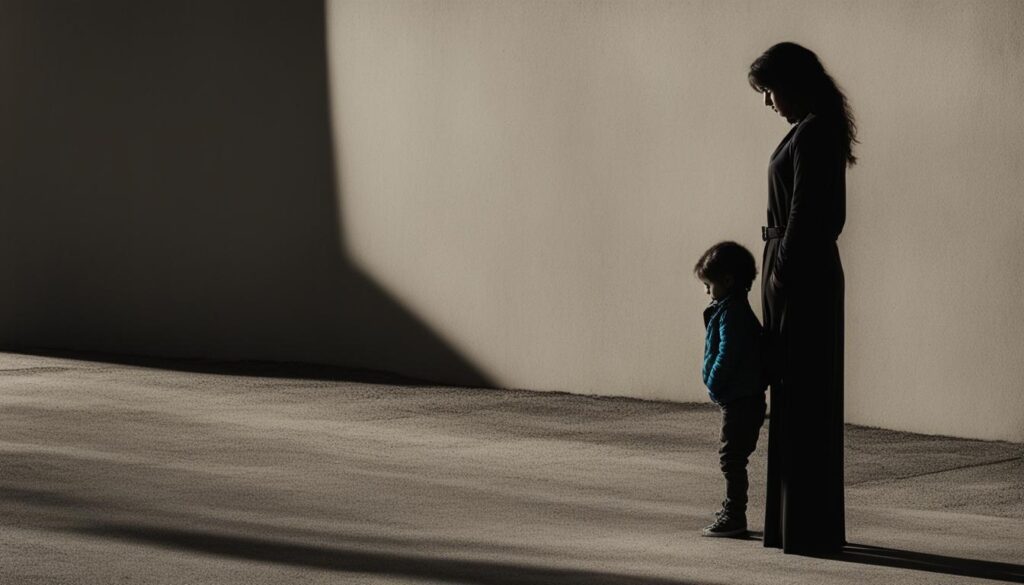
Were you aware that children of mothers diagnosed with Borderline Personality Disorder (BPD) are considered to be at significant risk? The impact of a borderline mother on family dynamics is deep and extensive.
Mothers with BPD often display oscillations between extreme forms of hostile control and passive aloofness in their interactions with their children. This unpredictable and unstable parenting style can have a significant impact on the emotional well-being and development of the child.
Key Takeaways
- Children of mothers with BPD are at a high risk of experiencing poor psychosocial outcomes.
- Mothers with BPD oscillate between extreme forms of hostile control and passive aloofness in their interactions with their children.
- Interventions such as attachment therapy and psychoeducational approaches are recommended for mothers and family members with BPD.
- Understanding the impact of maternal BPD on family dynamics is crucial for promoting healthy relationships within the family unit.
- Addressing the impact of BPD on child development can support the child’s overall well-being and growth.
Parenting Strategies of Mothers with BPD
Mothers with Borderline Personality Disorder (BPD) often utilize specific parenting strategies that can have a significant impact on their children’s well-being and development. Understanding these strategies is key to breaking the cycle of transmission of psychosocial vulnerability.
One unique aspect of parenting strategies employed by mothers with BPD is the oscillation between extreme forms of hostile control and passive aloofness in their interactions with their children. This volatile pattern can create instability and uncertainty for the child, affecting their emotional and psychological development.
It is crucial to delve into these parenting strategies and their effects in order to provide support and intervention that addresses the specific needs of both the mother and the child. By doing so, we can work towards promoting healthier family dynamics and reducing the transmission of vulnerability.
“Understanding the specific parenting strategies employed by mothers with BPD is crucial in breaking the cycle of transmission of psychosocial vulnerability.”
Parenting Strategies
In examining parenting strategies of mothers with BPD, it is important to note their tendency towards oscillations between hostile control and passive aloofness. In some instances, mothers with BPD may exhibit behaviors such as:
- Excessive criticism and emotional manipulation
- Inconsistent boundaries and inconsistent disciplinary practices
- Unpredictable emotional reactions
- Intense moments of closeness followed by withdrawal and detachment
These strategies can create an environment of uncertainty and emotional instability for the child. It is crucial to address these strategies and provide alternative approaches that foster healthy development and emotional well-being.
| Parenting Strategies | Effects on Children |
|---|---|
| Hostile Control | • Increased risk of anxiety and depression • Impaired self-esteem and self-identity |
| Passive Aloofness | • Feelings of abandonment and neglect • Difficulty forming secure attachments |
| Emotional Instability | • Emotional dysregulation • Difficulty managing stress and coping with emotions |
Note: The table above highlights some common parenting strategies of mothers with BPD and the potential effects on their children. It is important to remember that individual experiences may vary.
Understanding and addressing the parenting strategies of mothers with BPD is crucial for breaking the cycle of transmission of vulnerability. By providing support and intervention that promote healthy parenting practices, we can help create nurturing and stable environments for both mothers and their children.
Impact on Child Development
Children of mothers with Borderline Personality Disorder (BPD) may experience significant psychological effects that can have a lasting impact on their development. It is crucial to understand and address these effects in order to support their healthy growth and overall well-being.
One of the key psychological effects experienced by children of borderline mothers is emotional dysregulation. Due to the unpredictable and unstable nature of their mother’s emotions, these children may struggle with managing their own emotions effectively. This can lead to difficulties in forming healthy relationships, coping with stress, and regulating their own behavior.
Additionally, children of borderline mothers may also experience impaired self-identity. The fluctuating and inconsistent parenting behaviors exhibited by their mothers can make it challenging for these children to develop a stable sense of self. They may struggle with understanding their own emotions, values, and personal boundaries.
Cognitive disturbances are another common psychological effect on children of borderline mothers. The chaotic and invalidating environments in which these children grow up can hinder their cognitive development and lead to difficulties in academic performance, problem-solving, and decision-making.
Recognizing and addressing the impact of maternal BPD on child development is crucial for providing appropriate support and intervention. By implementing effective strategies to promote emotional regulation, strengthen self-identity, and enhance cognitive development, we can help these children overcome the psychological effects and thrive in their development.
| Psychological Effects on Children of Borderline Mothers |
|---|
| Emotional dysregulation |
| Impaired self-identity |
| Cognitive disturbances |

Gene-Environment Interaction in BPD
When it comes to understanding the development and transmission of Borderline Personality Disorder (BPD), researchers have discovered that it is influenced by both genetic and environmental factors. While there is a genetic predisposition to BPD, with heritability estimates ranging from 42% to 69%, environmental factors also play a significant role in shaping its manifestation.
The interplay between genetics and environment is crucial in comprehending the complexities of BPD. Let’s explore how gene-environment interaction, transgenerational transmission, and the heritability of BPD contribute to the understanding of this disorder.
The Genetic Predisposition
Research has consistently shown that BPD has a heritable component. Twin and family studies have revealed higher concordance rates among monozygotic twins compared to dizygotic twins, indicating that genetics play a significant role in BPD susceptibility. Heritability estimates between 42% and 69% suggest that genes account for a considerable proportion of BPD risk.
Although specific genes have yet to be identified, ongoing research aims to identify genetic variations associated with BPD susceptibility. Understanding the genetic underpinnings of BPD is crucial in unraveling its complex etiology and developing targeted interventions.
The Role of Environment
While genetics contribute to BPD, environmental factors also influence the development and expression of this disorder. Parenting styles, familial experiences, and other external factors can shape an individual’s vulnerability to BPD.
Children who grow up in invalidating environments, where their emotions and experiences are consistently dismissed or invalidated, may develop maladaptive coping mechanisms, emotional dysregulation, and an increased risk for BPD. In contrast, supportive and nurturing environments can provide a buffer against the development of BPD symptoms.
Understanding the interplay between genetics and environment is essential in comprehending the development and transmission of BPD.
Transgenerational Transmission
BPD can be passed down from one generation to another, highlighting the phenomenon of transgenerational transmission. This transmission occurs through a combination of genetic factors and environmental influences.
Children of mothers with BPD are at a higher risk of developing the disorder themselves. Not only do they inherit genetic vulnerabilities, but they are also exposed to the environmental factors associated with their mother’s BPD, such as invalidation and unstable family dynamics.
Breaking the cycle of transgenerational transmission requires a comprehensive understanding of the gene-environment interaction in BPD. By addressing both genetic predispositions and environmental factors, we can intervene at multiple levels to promote healthier outcomes for individuals and families affected by BPD.
| Genetic factors | Environmental factors |
|---|---|
| Heritability estimates ranging from 42% to 69% | Parenting styles |
| Twin and family studies | Family experiences |
| Transgenerational transmission | Invalidating environments |
The complex interplay between genetics and environment in BPD highlights the need for a holistic approach to understanding and addressing this disorder. By recognizing the genetic predisposition, environmental factors, and the transgenerational transmission of BPD, we can develop targeted interventions and support systems to promote better outcomes for individuals and families affected by this challenging condition.
Impact on Family Relationships
Family studies have revealed a strong familial aggregation of Borderline Personality Disorder (BPD), with its core features including affective instability and impulsivity. This means that there is a heightened risk of BPD occurring within families, affecting multiple individuals.
Relatives of individuals with BPD may also be more susceptible to related psychiatric disorders, further emphasizing the impact of familial aggregation. The presence of maternal BPD can have a profound effect on family relationships, leading to disruptions and challenges in maintaining healthy dynamics within the family unit.
Research has shown that the behavior and emotional instability exhibited by individuals with BPD can strain relationships and contribute to interpersonal conflicts and difficulties. The erratic mood swings, fear of abandonment, and impulsive actions characteristic of BPD can create an environment of instability and unpredictability within the family.
This can create a sense of unease and anxiety for family members, as they navigate the shifting dynamics caused by maternal BPD. The impact on family relationships extends beyond the immediate family unit, affecting extended family members as well.
It is important to understand and address the impact of maternal BPD on family relationships in order to provide appropriate support and intervention. By fostering a deeper understanding of BPD and its effects on family dynamics, we can work towards creating a supportive environment that promotes healing and growth for everyone involved.
Next, we will explore the outcomes and challenges faced during infancy and early childhood for children of mothers with BPD.
Outcomes during Infancy and Early Childhood
During the early stages of development, children of mothers with Borderline Personality Disorder (BPD) may experience a range of outcomes that can have lasting effects on their well-being. Research has shown that infants of mothers with BPD exhibit difficulties in regulating their emotions and display negative effects on early markers of self and emotion regulation skills.
This poor regulation of affect can impact socio-emotional development and overall well-being in early childhood. These early challenges in self and emotion regulation skills may persist and present long-term consequences for the child’s psychological and emotional development.

Understanding the impact of maternal BPD during infancy and early childhood is essential in providing appropriate support and intervention. By identifying and addressing these challenges, we can help promote healthy development and resilience in children at risk.
Spoiler Role in Family Dynamics
In dysfunctional family dynamics, the person with Borderline Personality Disorder (BPD) often plays the “spoiler” role. This role involves refusing to grow up, remaining dependent on the parent, and sabotaging or denigrating their efforts. The conflicting emotions and invalidating environments within the family contribute to the creation of BPD.
Dysfunctional family dynamics rooted in the “spoiler” role can have detrimental effects on the individual with BPD and the entire family unit. The constant tension, manipulation, and undermining of each other’s efforts create an invalidating environment that fosters emotional instability and disrupts healthy relationships.
“The ‘spoiler’ role perpetuates a cycle of dysfunction, hindering the growth and well-being of all family members.”
Furthermore, the “spoiler” role hinders the ability of the individual with BPD to develop a sense of responsibility, autonomy, and self-reliance. This dependency on the parent, even into adulthood, prevents the individual from developing their own identity and leads to a perpetuation of dysfunctional patterns within their own relationships.
It is crucial to address the impact of the “spoiler” role in family dynamics to break the cycle of dysfunction and create healthier relationships. By understanding the dynamics at play and implementing interventions focused on establishing healthy boundaries, promoting open communication, and fostering individual growth, we can promote positive change within the family system.
Next, we will explore the concept of invalidating environments and their role in the development of BPD.
Invalidating Environments and BPD
In families that produce individuals with BPD, we often observe the presence of invalidating environments, where parental invalidation is pervasive. The child grows up in an environment where their thoughts, feelings, and experiences are invalidated by their parents. This constant invalidation can have a profound impact on the child’s development and psychological well-being.
Parental invalidation involves dismissing, negating, or rejecting the child’s emotions, experiences, and self-expression. It sends the message that their feelings are not valid or important, leading the child to doubt their own reality. In such environments, the child often learns to give as good as they get, mirroring the invalidating behaviors they have experienced.
This cycle of invalidation can contribute to the development of psychosocial vulnerability in individuals with BPD. They may struggle with regulating their emotions and have difficulty maintaining healthy relationships. The constant invalidation impairs their ability to develop a secure sense of self and can lead to a heightened sensitivity to rejection and criticism.
The Impact of Invalidation on Emotional Regulation
The invalidation experienced in childhood can lead to significant difficulties in emotional regulation. Individuals who have grown up in invalidating environments may have a limited understanding of their own emotions and struggle to effectively express and manage them. This can result in frequent emotional outbursts, impulsivity, and unstable mood states.
The Impact on Interpersonal Relationships
Invalidation can also have a profound effect on an individual’s ability to form and maintain healthy relationships. The constant invalidation experienced in childhood can create a deep-seated fear of rejection and abandonment. As a result, individuals with BPD may engage in maladaptive behaviors in an attempt to avoid perceived rejection or gain validation from others.
“Growing up in an invalidating environment can shape how individuals with BPD perceive themselves and others.”
Invalidation can distort an individual’s perception of themselves and others. They may have difficulty trusting others and develop a fear of emotional intimacy. This can lead to tumultuous and unstable relationships characterized by intense emotions, idealization, and devaluation.
Psychotherapeutic Interventions
Psychotherapeutic interventions play a crucial role in addressing the impact of invalidation and promoting healing in individuals with BPD. Therapies such as Dialectical Behavior Therapy (DBT) focus on teaching emotional regulation skills, distress tolerance, and interpersonal effectiveness. These interventions provide individuals with BPD the tools they need to navigate the challenges of invalidation and establish healthier patterns of relating to themselves and others.
Effects of Invalidation on Individuals with BPD
| Effects of Invalidation | Impact |
|---|---|
| Impaired emotional regulation | Difficulty managing emotions |
| Difficulty forming and maintaining relationships | Trouble establishing trust and fear of rejection |
| Distorted self-perception | Low self-esteem and self-doubt |
| Heightened sensitivity to criticism | Strong emotional reactions to perceived rejection or criticism |

Addressing the impact of invalidating environments is crucial in supporting individuals with BPD on their journey to recovery. By providing validation, empathy, and promoting healthy coping mechanisms, we can help individuals break free from the cycle of invalidation and foster their psychosocial well-being.
Impact on Offspring’s Mental Health
The offspring of mothers with Borderline Personality Disorder (BPD) are at an increased risk for various mental health outcomes. One significant outcome is the development of borderline personality disorder itself. However, it is important to note that not all individuals with BPD have experienced adverse childhood experiences such as child abuse and neglect, which are commonly identified risk factors.
The impact of maternal BPD on the mental health of offspring needs to be addressed in order to provide appropriate support and intervention. By understanding the risk factors and potential psychosocial vulnerabilities, we can work towards promoting positive mental health outcomes for these individuals.
| Mental Health Outcome | Description |
|---|---|
| Borderline Personality Disorder | Offspring of mothers with BPD are at an increased risk of developing BPD themselves. |
| Depression | Offspring may experience depressive symptoms and have a higher likelihood of developing clinical depression. |
| Anxiety Disorders | There is a higher prevalence of anxiety disorders in offspring of mothers with BPD. |
| Substance Abuse | Offspring may be more susceptible to substance abuse and addiction. |
| Self-Harm | There is an increased risk of self-harming behaviors and suicide attempts in this population. |
It is crucial to provide support and intervention tailored to the unique needs of offspring of mothers with BPD. By addressing the risk factors and implementing appropriate strategies, we can aim to mitigate the negative mental health outcomes and promote overall well-being in these individuals.
Interventions and Treatment Recommendations
Treatment for mothers with Borderline Personality Disorder (BPD) should encompass a comprehensive approach that addresses the multifaceted nature of the disorder. In addition to individual therapy and medication management, interventions that target specific areas can be highly effective in promoting healthy family dynamics and supporting the child’s development.
Psychoeducation: Empowering Mothers with Knowledge
Psychoeducation plays a vital role in treatment for mothers with BPD. Providing mothers with a deep understanding of child development and recommended parenting practices equips them with essential tools and knowledge to navigate the complexities of parenting. By fostering insight into their own emotions and behaviors, mothers can effectively address the challenges associated with BPD and contribute to a stable and nurturing environment for their children.
Parenting Skills Training: Building Healthy Relationships
Parenting skills training interventions are designed to enhance the parenting abilities of mothers with BPD. Through structured guidance and support, these interventions focus on teaching mothers effective strategies for nurturing their child’s emotional, cognitive, and social development. By promoting positive parent-child interactions, these interventions can strengthen the bond between the mother and child, creating a foundation for healthy relationships.
“Parent-child interventions, such as attachment therapy and psychoeducational approaches, can be beneficial in promoting healthy family dynamics and supporting the child’s development.”
Attachment Therapy: Enhancing Parent-Child Bond
Attachment therapy is a specialized intervention that emphasizes the importance of secure parent-child relationships. By fostering a secure attachment bond, attachment therapy aims to enhance the child’s sense of safety and trust, ultimately promoting healthy socioemotional development. This intervention can help mothers with BPD develop attuned parenting skills and provide their children with a secure base from which to navigate the world.
Focusing on the Family System: Addressing the Impact of BPD
Interventions for mothers with BPD must take into account the impact of the disorder on the entire family system. By involving family members in the treatment process, therapists can help them understand BPD, manage their own emotions, and develop effective communication skills. Family therapy can serve as a supportive environment for family members to express their concerns, improve understanding, and foster healthy dynamics within the family unit.

Support for Families and Relatives
Psychoeducational programs and family support play a crucial role in helping families and relatives navigate the challenges of living with a loved one who has Borderline Personality Disorder (BPD). These programs provide valuable education on BPD, effective communication techniques, and strategies for managing difficult behaviors.
When a family member is diagnosed with BPD, it can be overwhelming for everyone involved. Family support groups offer a safe space for sharing experiences, gaining insights, and receiving emotional support from others who understand the unique challenges of living with BPD.
Psychoeducational programs equip families and relatives with the knowledge and tools to better understand BPD, its symptoms, and its impact on relationships. By increasing awareness and promoting empathy, these programs foster healthier family dynamics and strengthen bonds of understanding and acceptance.
“Family support and psychoeducation are essential elements in the journey of supporting a loved one with BPD. These programs provide valuable resources, guidance, and validation for family members and relatives, empowering them to better navigate the complexities of the disorder.”
Furthermore, psychoeducational programs can help families and relatives develop effective coping strategies, enhance communication skills, and establish boundaries that promote emotional well-being for both the individual with BPD and their loved ones. By equipping families with the tools to manage challenging situations and promote a supportive environment, these programs contribute to the overall well-being of everyone involved.
It is also important to recognize that relatives of individuals with BPD may experience their own emotional challenges and may benefit from individual therapy or support groups tailored specifically to their needs. By addressing the unique needs and experiences of relatives, these resources provide a supportive network that fosters personal growth and resilience.
Ultimately, family support and psychoeducational programs create a nurturing and understanding environment where individuals with BPD and their loved ones can learn, heal, and grow together.
Benefits of Psychoeducational Programs and Family Support for Relatives of Individuals with BPD
| Benefits | Description |
|---|---|
| Increased understanding | Educational programs provide knowledge about BPD, its symptoms, and its impact on relationships, helping relatives gain a deeper understanding of their loved one’s experiences. |
| Improved communication | Psychoeducational programs equip relatives with effective communication techniques that promote open dialogue, empathy, and healthy boundaries. |
| Enhanced coping strategies | Relatives learn valuable coping strategies to manage challenging behaviors and emotional situations, promoting their own well-being and resilience. |
| Validation and support | Family support groups offer a sense of validation and understanding through the shared experiences, challenges, and triumphs of participants. |
| Promoted well-being | By fostering healthier family dynamics and nurturing supportive environments, relatives can experience improved emotional well-being and stronger relationships. |
Conclusion
The impact of maternal Borderline Personality Disorder (BPD) on children and family dynamics is significant. Children of mothers with BPD are at a high risk of experiencing poor psychosocial outcomes and facing unique challenges in their development. It is crucial to understand the parenting strategies, gene-environment interaction, and the impact on family dynamics in order to provide appropriate support and intervention.
By addressing these factors, we can strive to create healthier family dynamics and promote positive child development. Interventions such as attachment therapy and psychoeducational approaches can be instrumental in promoting healthy family relationships and supporting the child’s well-being. Additionally, providing psychoeducation regarding child development and recommended parenting practices to mothers with BPD is essential.
Overall, recognizing the impact of maternal BPD on family dynamics and child development is crucial to ensure the well-being of both the mother and the child. By providing the necessary support and intervention, we can help these families navigate the challenges they face and promote positive outcomes for the children affected by maternal BPD.
FAQ
What is the impact of a borderline mother on family dynamics?
Mothers with Borderline Personality Disorder (BPD) can have a profound impact on family dynamics, often displaying oscillations between extreme forms of hostile control and passive aloofness in their interactions with their children. This can create disruptions and challenges within the family unit.
What are the parenting strategies of mothers with BPD?
Mothers with BPD may employ parenting strategies characterized by oscillations between extreme forms of hostile control and passive aloofness. These strategies can contribute to the transmission of vulnerability to their offspring and impact the development of psychosocial outcomes.
How does maternal BPD impact child development?
Children of mothers with BPD may experience psychological effects that can impact their development. These effects can manifest in emotional dysregulation, impaired self-identity, and cognitive disturbances, which can have long-lasting consequences.
Is there a gene-environment interaction in BPD?
Yes, there is evidence of a gene-environment interaction in the development of BPD. While BPD has a genetic predisposition, environmental factors such as parenting styles and familial experiences also play a significant role in the development and transmission of BPD.
What is the impact of maternal BPD on family relationships?
Maternal BPD can have a significant impact on family relationships, with potential disruptions and challenges in maintaining healthy dynamics within the family unit. There is a strong familial aggregation of BPD and its core features, which can affect the well-being of family members.
What are the outcomes during infancy and early childhood for children of mothers with BPD?
Studies have found evidence of poor regulation of affect and negative effects on early markers of self and emotion regulation skills in infants of mothers with BPD. These early experiences can have implications for socio-emotional development and overall well-being.
What is the “spoiler” role in family dynamics?
The “spoiler” role refers to the role played by the person with BPD within the family dynamics. This role involves refusing to grow up, remaining dependent on the parent, and sabotaging or denigrating their efforts. Dysfunctional family dynamics and conflicting emotions can contribute to the development of BPD.
How do invalidating environments impact the development of BPD?
In families that produce individuals with BPD, invalidation by parents is pervasive. The child learns to mirror the invalidating behaviors they have experienced, contributing to the development of psychosocial vulnerability and difficulty regulating emotions and maintaining healthy relationships.
What are the impacts of maternal BPD on offspring’s mental health?
Offspring of mothers with BPD are at increased risk for various mental health outcomes, including borderline personality disorder itself. While child abuse and neglect are commonly identified risk factors, not all individuals with BPD have experienced these adverse childhood experiences.
What interventions and treatments are recommended for mothers with BPD?
Treatment for mothers with BPD should include psychoeducation regarding child development and recommended parenting practices. Parent-child interventions, such as attachment therapy and psychoeducational approaches, can be beneficial in promoting healthy family dynamics and supporting the child’s development.
How can families and relatives receive support when living with an individual with BPD?
Psychoeducational programs and family support can play a significant role in assisting families and relatives in understanding and coping with the challenges of living with an individual with BPD. These programs provide education on BPD, communication techniques, and strategies for managing difficult behaviors.
What is the impact of maternal BPD on family dynamics and child development?
The impact of maternal BPD on family dynamics and child development is profound. Children of mothers with BPD are at a high risk of experiencing poor psychosocial outcomes, and the interaction between parenting strategies, gene-environment influences, and family dynamics can significantly impact their well-being.









